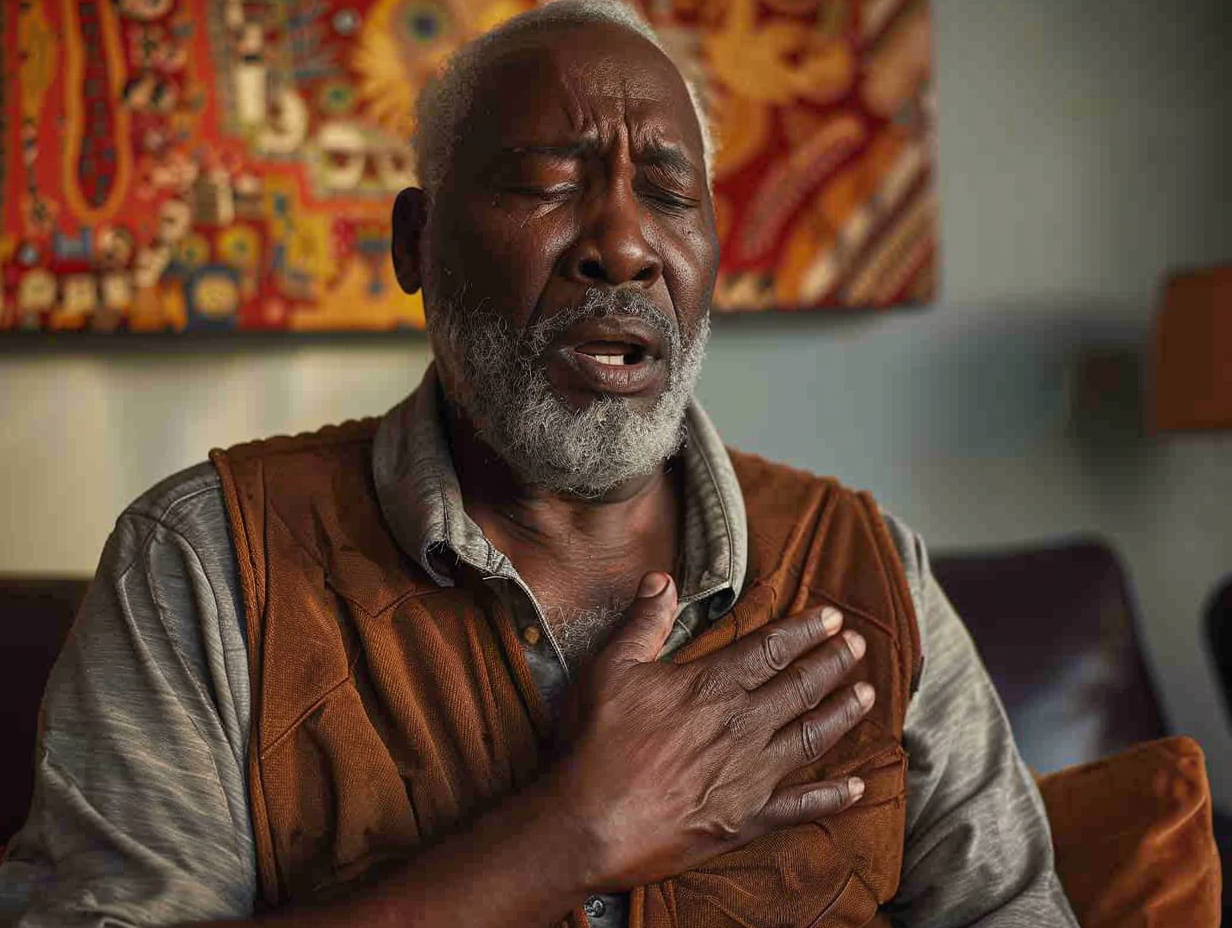
Heart failure, a serious condition where the heart is unable to pump blood efficiently, disproportionately impacts the Black community. While many factors contribute to heart failure, certain medications can increase the risk. Understanding these medications and their effects is crucial for prevention and management. This article explores various medications that can cause heart failure, providing valuable insights for patients and healthcare providers.
Understanding heart failure
Heart failure, also known as congestive heart failure (CHF), occurs when the heart cannot pump enough blood to meet the body’s needs. This can result from conditions that overwork or damage the heart, such as high blood pressure, coronary artery disease, and diabetes. Symptoms include shortness of breath, fatigue, swelling in the legs, and rapid or irregular heartbeat.
Medications linked to heart failure
Several classes of medications have been identified as potential contributors to heart failure. These medications can either directly harm the heart muscle or exacerbate existing conditions that lead to heart failure.
1. Non-steroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, commonly used to relieve pain and inflammation, can have adverse effects on heart health. Medications such as ibuprofen and naproxen can lead to fluid retention, increased blood pressure, and, ultimately, heart failure. Long-term use of NSAIDs, particularly at high doses, is associated with an elevated risk of heart failure.
Key points:
- NSAIDs can cause fluid retention and increased blood pressure.
- Long-term, high-dose use increases heart failure risk.
2. Diabetes medications
Some diabetes medications, particularly thiazolidinediones (TZDs) like rosiglitazone and pioglitazone, have been linked to an increased risk of heart failure. These drugs can cause fluid retention and weight gain, which can amplify heart failure symptoms. Patients with pre-existing heart conditions should use these medications cautiously.
Key points:
- TZDs can cause fluid retention and weight gain.
- Increased heart failure risk in patients with existing heart conditions.
3. Chemotherapy agents
Chemotherapy drugs, such as anthracyclines (doxorubicin, daunorubicin), can be cardiotoxic, leading to heart muscle damage and heart failure. These drugs are essential for treating cancer but require careful monitoring of heart function during and after treatment to prevent severe cardiac complications.
Key points:
- Anthracyclines can damage heart muscle.
- Monitoring heart function during chemotherapy is crucial.
Additional medications affecting heart health
Apart from the major categories discussed, other medications can also negatively impact heart health.
4. Antihypertensive drugs
While antihypertensive drugs are essential for managing high blood pressure, some can adversely affect heart function. For instance, beta-blockers can sometimes lead to heart failure if not properly managed. However, when used correctly, they are beneficial for heart failure treatment.
Key points:
- Some antihypertensives can affect heart function negatively.
- Proper management is crucial for safety and efficacy.
5. Antiarrhythmic medications
Antiarrhythmic drugs, used to treat irregular heartbeats, can sometimes worsen heart failure. Drugs like flecainide and propafenone are associated with increased heart failure risk, particularly in patients with existing heart conditions. Monitoring and adjusting these medications is vital to prevent complications.
Key points:
- Antiarrhythmics can worsen heart failure.
- Careful monitoring and adjustment are necessary.
Managing medication-induced heart failure
Preventing heart failure involves understanding the risks associated with certain medications and taking proactive steps to mitigate them. Here are some strategies for managing and preventing medication-induced heart failure:
Regular monitoring: Regular monitoring of heart function, particularly for patients taking high-risk medications, is crucial. Monitoring includes routine check-ups, echocardiograms, and blood tests to detect early signs of heart dysfunction.
Medication review: Healthcare providers should regularly review patients’ medications to identify potential risks and make necessary adjustments. This is especially important for patients with multiple prescriptions or those taking high-risk drugs.
Lifestyle modifications: Adopting a heart-healthy lifestyle can significantly reduce the risk of heart failure. This includes maintaining a balanced diet, regular exercise, avoiding smoking, and managing stress. These lifestyle changes can complement medical treatments and improve overall heart health.
Conclusion
Understanding the link between certain medications and heart failure is essential for prevention and management. Awareness of the risks associated with certain medications enables patients and healthcare providers to take proactive steps to minimize risk. By recognizing these risks, individuals can make informed decisions about their treatment options and work closely with their healthcare team to monitor heart health.
Regular monitoring of heart function, including routine check-ups and diagnostic tests, is crucial for detecting early signs of heart dysfunction. Medication reviews are essential for identifying and addressing potential risks and ensuring that patients receive the safest and most effective treatment. Additionally, adopting a heart-healthy lifestyle, which includes a balanced diet, regular exercise, smoking cessation, and stress management, can significantly reduce the risk of heart failure and improve overall heart health.
By understanding the potential risks and taking appropriate measures, patients can protect their heart health and reduce the likelihood of heart failure. With the right approach, it is possible to manage medications effectively while safeguarding heart health.
This story was created using AI technology.